If your patient is exhibiting symptoms of unexplained exhaustion, gastrointestinal distress, or even psychosis, and you cannot identify a cause, you may be dealing with a chronic infection. Chronic infections can be viral, bacterial, fungal, or parasitic in nature.
Some examples include HIV, tuberculosis, and hepatitis. Chronic infections can also include sinus, yeast, or ear infections. Lyme disease and joint pain can likewise be caused by active long-term infections.
So how do we test for chronic infections, determine who is at risk and decide on treatment strategies? We asked an expert in diagnosing and treating chronic infection, Dr Carissa Doherty ND.
Dr Doherty is a naturopathic doctor who opened her natural care clinic in Burlington almost 20 years ago. Her approach in treating chronic illness has become world renowned and draws patients from all over the globe.
Key Take-Aways
Defining a chronic infection
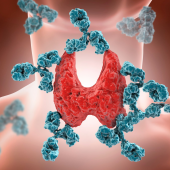
Anytime an infection occurs, the immune system identifies and kills it. A chronic infection occurs when that process does not happen; the infection stays alive.
Presentation of chronic infection
Ear infections, chronic strep, and yeast infections are common examples of chronic infections. Symptoms may reoccur every 4 to 6 weeks, thus you have a cyclic type of symptom pop up that can be a chronic infection. While more typical in children, chronic infections also occur in adults.
Lyme disease as a chronic infection
It is important to rule out Lyme disease when considering chronic infection symptomology because this disorder is hard to treat. Lyme disease has a long disease progression and affinity for deep tissues.
Testing for chronic infection
Instead of testing for an active infection, what is recommended is to look for past exposure patterns. Recent exposure testing is not accurate without looking at patterns over the last two months or longer. Tissues to be tested include urine, sputum, blood and stool.
Treatment of chronic infection
Start with the “kill protocol” which includes doses of herbs, sometimes at higher dosage levels, even in children. While medical doctors cannot give drugs in high doses because it is dangerous, naturopathic practitioners can prescribe high doses of antibacterial agents such as herbs because there is seldom an issue with overdose.
Specific treatment options
For viral killing, vitamin A, vitamin D, St John's Wort, zinc, oregano oil, berberine, and black cumin are recommended. Bacterial killers include black cumin, berberine, zinc, oregano, oil, curcumin, and even stevia as the sweetener can act like an anti-biofilm agent.
For yeast infections, garlic, oregano oil, neem and Artemisia annua are effective treatment options.
St John’s Wort
St John's Wort is a good choice for chronic viral infections, particularly for viral biofilms. Defaulting to St John's Wort as an antiviral, antibacterial, and antifungal, working in a biofilm configuration, can be a useful treatment.
Chronic infection of the gut
The large and small intestines are sites of chronic infection, but typically not the stomach because it is very acidic. Often these infections will involve biofilms found with situations of fecal loading. The strategy is to penetrate the calcified layer where the infection is manifesting itself.
Treating chronic gut infections
Recommended treatments include an oral osmotic diarrhea inducing agent. The water influx will flush the intestine. You do not want to perturb peristalsis because that will cause harm in the system. The idea is you put water from the rest of your body into the intestinal lumen and slowly pull the resultant debris off over time.
Magnesium oxide
Magnesium oxide is effective for chronic infection linked to constipation. A single teaspoon dose is considered a small dose in an adult population, but an aggressive dose for a child. A suggested daily dose is 6000 mg which is about a teaspoon. Adults can be given as high as 10000 mg a day.
Disadvantages of antibiotics
Antibiotics will make biofilms up to 20 times stronger, as the biofilm walls will become more robust. Antibiotics then cannot penetrate the biofilm. In fact, the biofilm becomes so irritated that it will send the signal inside the biofilm, so that all the microbes, even made up of different strains like viruses and bacteria in the same location, drop their cell wall, exchange DNA internally, and thus become smarter.
Key Quotes
“Another term for that is a biofilm. So, there's three individuals in this scenario. There's you, the individual, there's the infection and the microbes. So, biofilm is single-celled organisms working as a unit all together, kind of like coral in the ocean.”
Dr Carissa Doherty
==
The opinions expressed in this Nutramedica program are those of the guests and contributors. They do not necessarily reflect the opinions of Nutritional Fundamentals For Health Inc.
This video is intended for licensed or registered health professionals and students of health professions only. These statements have not been evaluated by the Food and Drug Administration. Information contained in these programs are not intended to diagnose, treat, cure or prevent any disease.